About
Venous thromboembolism (VTE), including DVT, PE and arterial thromboembolism, are all common, costly, and contribute to substantial patient morbidity and mortality. Despite the availability of society guidelines and other data, VTE is commonly mismanaged.(1-4) Several provider and system factors may contribute to this discrepancy, including lack of provider education and guidelines which may be inaccessible, infrequently updated, or cumbersome to navigate.
Our group aims to address this issue by curating an easily-accessible, up-to-date, evidence-based, and streamlined set of guidelines for managing common issues in the domains of thrombosis and hemostasis. Inspired by guidelines for the management of malignancy published by the National Cancer Center Network (NCCN), our guidelines are similarly designed with fluidity and visual simplicity in mind. Our guidelines are primarily adapted from data published by CHEST, with supplemental pertinent high-quality, high-impact data whenever available.
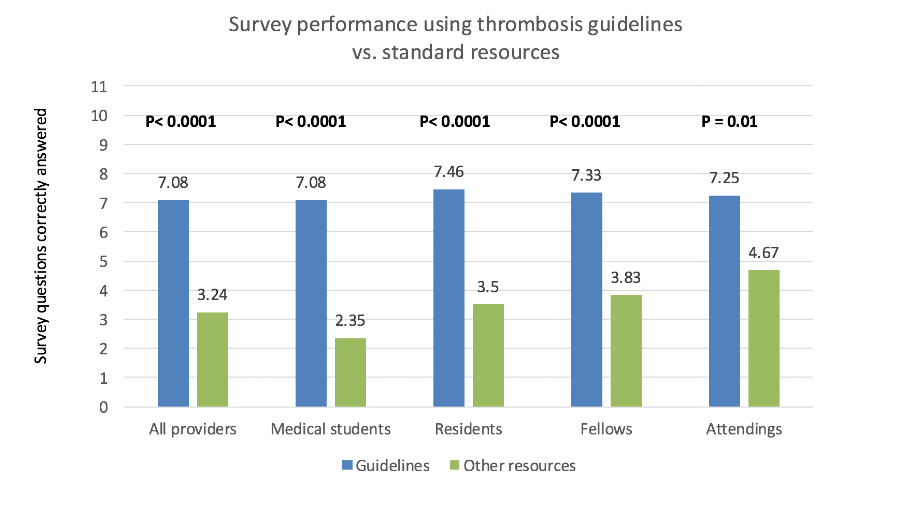
In a prospective, single-center, web-based study, our thrombosis guidelines led to statistically significantly greater number of correct answers to common clinical scenarios related to thrombosis and hemostasis across all levels of training (see figure below). This data was presented at the American Society of Hematology 2016 annual meeting.
American Society of Hematology 2016 annual meeting, San Diego CA
1. Caprini JA, Tapson VF, Hyers TM, et al. Treatment of venous thromboembolism: Adherence to guidelines and impact of physician knowledge, attitudes, and beliefs. Journal of Vascular Surgery. 2005;42(4):726-733
2. Meyer MR, Witt DM, Delate T, et al. Thrombophilia testing patterns amongst patients with acute venous thromboembolism. Thromb Res. 2015;136(6):1160-1164
3. Sudarmana A, Monagle P. Thrombophilia testing in a tertiary paediatric hospital: Indications, outcomes and appropriateness. J Paediatr Child Health. 2015;51(10):1017-1022
4. Shen Y-M, Tsai J, Taiwo E, et al. Analysis of Thrombophilia Test Ordering Practices at an Academic Center: A Proposal for Appropriate Testing to Reduce Harm and Cost. PLoS ONE. 2016;11(5):e0155326